[ad_1]
In a recent study published in the journal proceedings of the National Academy of SciencesResearchers analyzed the inflammatory capacity of fragmented components of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Intense research during the coronavirus disease 2019 (COVID-19) pandemic has helped understand SARS-CoV-2 infection. However, it is still unclear what makes the virus capable of provoking a dangerous inflammatory response. Research has suggested that amphiphilic cationic peptides of the innate immune system assemble in an amyloid-like manner with anionic nucleic acids and form pro-inflammatory complexes.
 Study: Beyond viral: SARS-CoV-2 as a reservoir of immunomimetic peptides that reassemble into proinflammatory supramolecular complexes. Image credit: NIAID
Study: Beyond viral: SARS-CoV-2 as a reservoir of immunomimetic peptides that reassemble into proinflammatory supramolecular complexes. Image credit: NIAID
The study and the findings.
The present study investigated whether SARS-CoV-2 cleaved peptides assemble with anionic double-stranded RNA (dsRNA) into supramolecular complexes. The viral proteome was considered a reservoir of peptide fragments that are released upon proteolytic destruction of virions. The researchers leveraged a support vector machine (SVM) classifier to recognize antimicrobial peptide (AMP)-like sequences (xenoAMP) in the SARS-CoV-2 proteome.
Viral protein sequences were scanned across a sliding window of 24 to 34 amino acids to identify potential xenoAMPs and test whether they behave like AMPs if cleaved at different positions. Sequences were selected based on the output provided by the classifier as a sigma (σ) score, where a strongly positive score implied that the sequence was very likely to be an AMP.
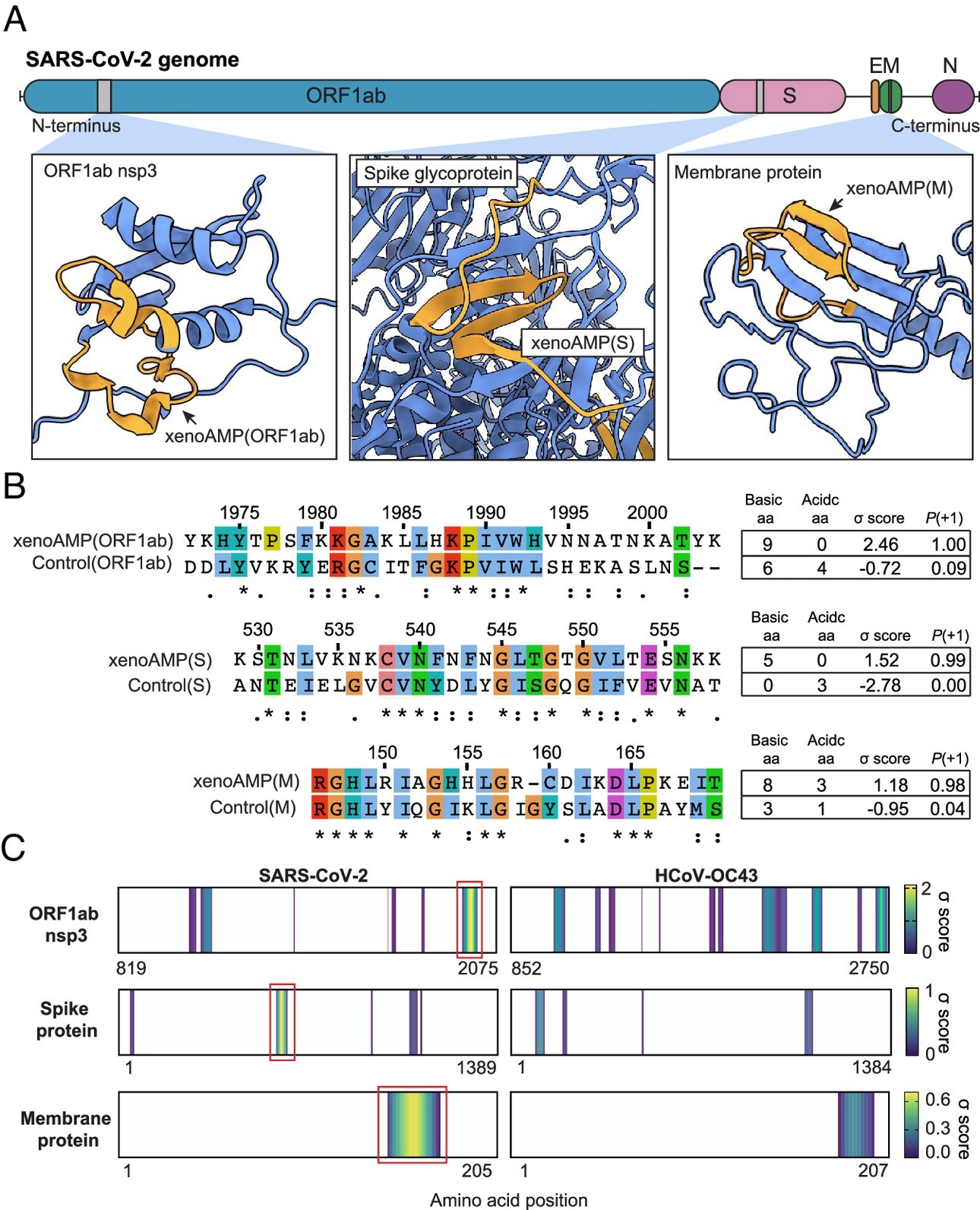
Existence of exogenous host proinflammatory antimicrobial peptide (xenoAMP) mimics in SARS-CoV-2 proteins. (A) SARS-CoV-2 proteins are scanned with a machine learning AMP classifier. Each query sequence is assigned a score σ that measures its AMP character. Three representative high-scoring sequences are studied: xenoAMP(ORF1ab), xenoAMP(S) and xenoAMP(M). Gray bars mark the location where the corresponding sequences are selected. (B) SARS-CoV-2 sequences are aligned and compared to their counterparts in a human common cold coronavirus HCoV-OC43: Control (ORF1ab), Control(S), and Control(M). Asterisks, colons, and dots indicate positions that have completely conserved residues, those that have very similar properties, and those that have weakly similar properties, respectively. Color is assigned to each residue using the ClustalX scheme. (C) σ-score heatmaps compare the distribution of high-scoring sequences in three proteins from SARS-CoV-2 and HCoV-OC43. The first amino acid of each sequence is colored according to its average σ score; regions with negative average σ scores (non-AMP) are colored white. “Hot spot” clusters of high-scoring sequences for SARS-CoV-2 (bright yellow regions in brackets in red boxes) have consistently higher scores and span broader regions of sequence space compared to HCoV-OC43 . This trend suggests that hot spots in SARS-CoV-2 may generate higher scoring sequences for a greater diversity of enzymatic cleavage sites than those in HCoV-OC43.
Additionally, the team selected specific sequences from this population of (high-scoring) sequences with a high cationic charge. Specifically, they focused on prototypical candidates for membrane protein (M), spike protein (S), and open reading frame 1ab (ORF1ab) polyprotein. in silicon The analyzes showed that these xenoAMPs could be generated during proteasomal degradation, with matrix metalloproteinase 9 (MMP9) and neutrophil elastase (NE) capable of generating them.
The team next compared the SARS-CoV-2 xenoAMPs with homologous sequences from SARS-CoV-1 and non-pandemic human CoVs. This showed that the sequences were partially conserved. A comparison of the σ-score heatmaps of ORF1ab, S, and M proteins between SARS-CoV-2 and HCoV-OC43 revealed that high-scoring sequences clustered into hotspots, and that SARS hotspots -CoV-2 had higher scores and spanned broader regions. than those of HCoV-OC43.
Additionally, mass spectrometry was performed on tracheal aspirate samples from patients with severe COVID-19. The team detected fragments of the host AMP, cathelicidin LL-37, in 20 samples (out of 29). In contrast, 28 samples contained viral peptide fragments, some of which had σ scores high enough to qualify as xenoAMP.
The three xenoAMPs, xenoAMP(S), xenoAMP(M), and xenoAMP(ORF1ab), were experimentally observed to accompany and assemble with dsRNA into LL-37-like complexes. Polyinosine:polycytidylic acid (poly(I:C) was used as a synthetic analogue to mimic the viral dsRNA generated during replication. The structures of the xenoAMPs-poly(I:C) complexes were similar to the host AMPs-dsRNA complexes.
The team next investigated the robustness of these self-assembled pro-inflammatory complexes under non-optimal conditions. They found that nanocrystalline structures were preserved when the participating xenoAMPs were shortened. Furthermore, SARS-CoV-2 xenoAMPs were found to cocrystallize with LL-37, suggesting that host AMPs and xenoAMPs could synergistically activate inflammatory responses.
The immune activation capacity of SARS-CoV-2 xenoAMPs was compared with that of HCoV-OC43 homologous peptides using human monocytes. Monocytes treated with xenoAMP-poly(I:C) released 1.7-fold more interleukin (IL)-8 than poly(I:C)-treated controls. In contrast, complexes formed with HCoV-OC43 homologous peptides induced much lower IL-8 levels.
Furthermore, xenoAMP-poly(I:C) stimulation of primary human dermal microvascular endothelial cells (HDMVEC) triggered robust IL-6 production, which was not observed with complexes formed from HCoV-OC peptides43. Notably, HDMVECs treated with xenoAMP-poly(I:C) showed significant upregulation of several proinflammatory cytokine and chemokine genes.
Finally, the researchers measured the immune activation capacity in mice. Naïve C57BL/6 mice were treated with xenoAMP(ORF1ab)-poly(I:C) complexes or poly(I:C) alone (control). Treatment with xenoAMP(ORF1ab)-poly(I:C) increased plasma levels of IL-6 and CXC motif chemokine ligand 1 (CXCL1) by 1.6- and 2.2-fold, respectively, compared with poly(I:C) alone. Furthermore, IL-6 and CXCL1 levels increased 1.2-fold in the lung compared to control treatment.
Conclusions
In summary, the study has illustrated an unexpected mechanism of inflammation spreading through uninfected cells in COVID-19, in which viral fragments mimic AMPs such as LL-37. This could be important for understanding why the host immune system in COVID-19 resembles that of people with autoimmune conditions such as rheumatoid arthritis and lupus.
The researchers found that host proteases could generate xenoAMP, suggesting that protease inhibitors that suppress xenoAMP generation could have a clinical impact on virus-induced inflammation. The proteolytic degradation of SARS-CoV-2 could differ between host individuals, possibly explaining the heterogeneity of infection outcomes, for example, asymptomatic and fatal.

